Drug Price Comparison Calculator
Compare Drug Prices Across Countries
This tool demonstrates the massive price differences for life-saving medications between the U.S. and other countries. Based on the AbbVie scandal analysis.
Why the huge price difference?
US drug pricing lacks negotiation (Medicare can't negotiate), while countries like Canada and the UK use government price controls. AbbVie's patent tactics and offshore manufacturing also contribute to these disparities.
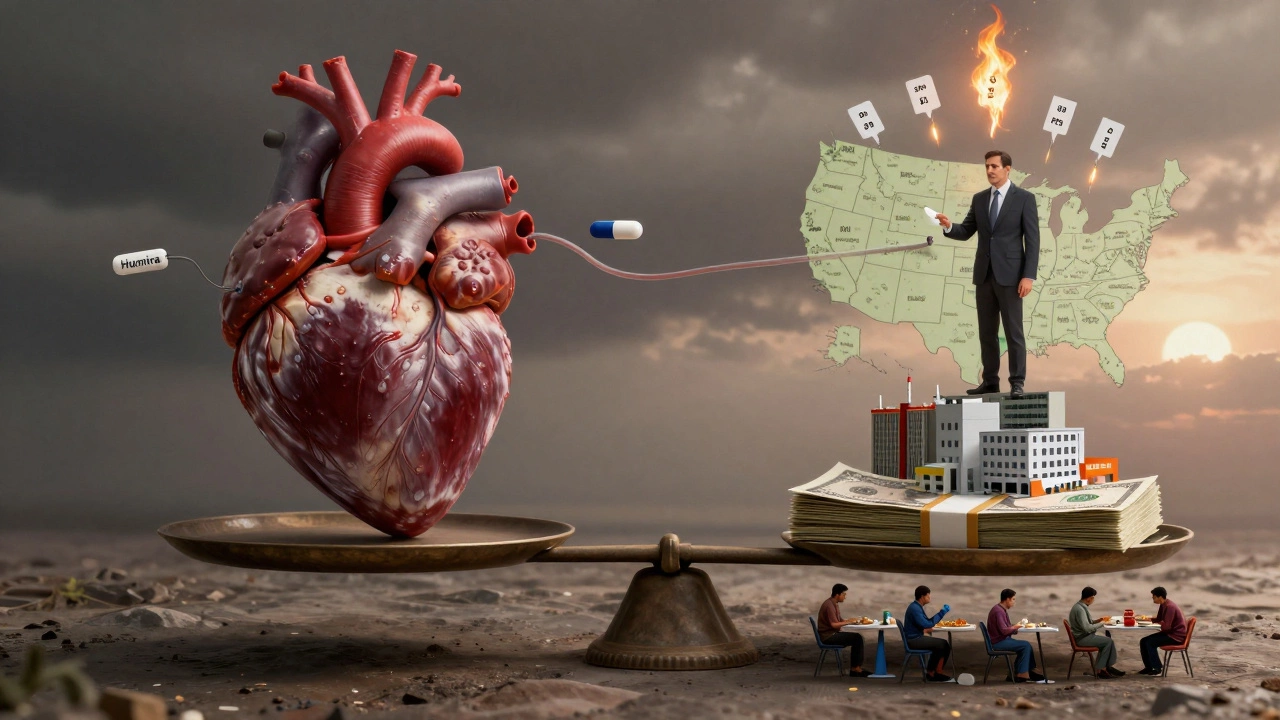
AbbVie didn’t become one of the world’s biggest pharmaceutical companies by accident. But behind its billion-dollar profits and blockbuster drugs like Humira lies a string of controversies that have shaken regulators, patients, and lawmakers alike. The AbbVie scandal isn’t one single event-it’s a pattern. A pattern of aggressive pricing, legal maneuvering, and offshore manufacturing that puts profits ahead of access.
How Humira became a cash machine
Humira, AbbVie’s flagship drug for autoimmune diseases like rheumatoid arthritis and Crohn’s, hit the market in 2003. By 2020, it was the best-selling drug in history, bringing in over $21 billion in a single year. That’s more than the GDP of 120 countries. But here’s the problem: Humira’s active ingredient, adalimumab, was developed in the 1990s. The original patent expired years ago. So how did AbbVie keep charging $7,000 per dose in the U.S. while other countries paid under $500?
The answer? Patent thickets. AbbVie filed over 100 patents on Humira-not for new medical breakthroughs, but for minor changes in delivery methods, packaging, and dosing schedules. Each patent delayed generic competition. The FDA approved the first biosimilar in 2023, but AbbVie’s legal battles pushed market entry back by nearly two years. Patients paid the price. In 2022, U.S. Medicare spent over $4.3 billion on Humira alone. That’s $1,200 per patient per month. Many patients skipped doses or split pills to make it last.
Offshore manufacturing and the India connection
AbbVie doesn’t manufacture Humira in the U.S. Most of its active pharmaceutical ingredients (API) come from India. Specifically, from contract manufacturers in Gujarat and Hyderabad. These facilities supply raw materials to AbbVie’s global supply chain. But here’s where things get murky.
In 2021, the U.S. FDA issued a warning letter to an AbbVie supplier in India after inspectors found serious violations: contaminated equipment, unverified raw materials, and falsified lab records. The facility was shut down. AbbVie didn’t disclose the issue publicly. Instead, it quietly shifted production to another Indian plant. That plant, too, had prior violations. The FDA flagged it in 2018 for failing to properly validate cleaning procedures. No one outside the industry knew. Patients had no idea their life-saving drug was being made under conditions that broke U.S. safety rules.
AbbVie’s Indian suppliers are not outliers. They’re part of a system. India produces over 60% of the world’s generic drugs and 40% of the APIs used in U.S. medications. But oversight is thin. Regulatory inspections by the FDA are rare-only 10% of Indian manufacturing sites are inspected every five years. AbbVie’s reliance on this system isn’t a mistake. It’s a strategy. Lower labor costs, looser enforcement, and fewer regulatory hurdles mean higher margins.

The price gap between countries
Look at the numbers. In Canada, a 30-day supply of Humira costs $180. In the UK, under the NHS, it’s $110. In India, generic versions sell for under $15. But in the U.S., without insurance, the price is $7,200. Why? Because U.S. law doesn’t allow Medicare to negotiate drug prices. And because AbbVie’s legal team has spent over $200 million on lobbying since 2015 to block price controls.
Meanwhile, AbbVie’s R&D spending on new drugs has dropped. In 2020, only 12% of its R&D budget went to new molecular entities. The rest? Extending patents, marketing, and legal fees. In 2023, AbbVie’s CEO received $24 million in total compensation. That same year, over 1.2 million Americans couldn’t afford their Humira prescriptions. Some turned to online pharmacies in Mexico. Others used crowdfunding to pay for treatment.
Legal battles and public backlash
It wasn’t until 2024 that the U.S. Senate launched a formal investigation into AbbVie’s pricing practices. The report found evidence of "systemic abuse" of the patent system. The Justice Department opened a probe into whether AbbVie engaged in anti-competitive behavior. Three class-action lawsuits are now moving through federal courts. One, filed by the State of California, claims AbbVie colluded with pharmacy benefit managers to block generics.
Public anger has grown. Patient advocacy groups have started #HumiraJustice campaigns. In 2025, a documentary called "The $7,000 Pill" aired on PBS, showing interviews with patients who lost jobs because they couldn’t afford co-pays. The backlash forced AbbVie to announce a patient assistance program-but only for those earning under $50,000 a year. Millions still fall through the cracks.
What’s next for AbbVie and the industry?
AbbVie’s next big drug, Rinvoq, is already facing the same pattern. Patent extensions. Price hikes. Limited transparency. The company claims it needs high prices to fund innovation. But data shows otherwise. Between 2015 and 2024, AbbVie spent $28 billion on stock buybacks and dividends. It spent $11 billion on R&D.
The real scandal isn’t just about one company. It’s about a system that lets pharmaceutical giants turn life-saving drugs into financial instruments. India’s role in this isn’t accidental. It’s structural. The U.S. outsources manufacturing to cut costs, then blames foreign suppliers when things go wrong. Meanwhile, patients pay the highest prices in the world.
Until Congress forces drug price transparency, ends patent abuse, and requires full disclosure of manufacturing locations, the AbbVie scandal won’t be an exception. It’ll be the rule.
Did AbbVie break the law?
AbbVie hasn’t been criminally convicted, but multiple federal investigations are ongoing. The U.S. Senate found evidence of anti-competitive behavior, and the Justice Department is reviewing whether AbbVie violated antitrust laws by delaying generic competition. Several states have filed civil lawsuits alleging fraud and price gouging. Legal experts say the company’s patent strategy may be within legal bounds-but it’s widely seen as unethical.
Why is AbbVie’s manufacturing in India a problem?
AbbVie relies on Indian manufacturers because they’re cheaper. But several of these suppliers have been flagged by the FDA for poor quality control, falsified records, and unsanitary conditions. The U.S. government doesn’t inspect most of these plants regularly. So while AbbVie markets Humira as a safe, high-quality drug, its raw ingredients often come from facilities with known violations. Patients are unaware of this gap between marketing and reality.
Can I get a cheaper version of Humira in India?
Yes. Generic versions of adalimumab (the active ingredient in Humira) are sold legally in India for under $15 per month. But importing them into the U.S. is illegal under federal law, even if they’re identical in quality. Some patients do it anyway through online pharmacies, risking fines or confiscation. The FDA doesn’t regulate these imports, so safety can’t be guaranteed.
Is AbbVie the only company doing this?
No. Other drugmakers like Pfizer, Johnson & Johnson, and Roche have used similar tactics-extending patents, delaying generics, and shifting manufacturing overseas. But AbbVie is the most extreme example. Humira was its single biggest product for over a decade, and its profit margins were among the highest in pharmaceutical history. No other drug has generated so much revenue while facing so much public scrutiny.
What’s being done to fix this?
In 2022, the Inflation Reduction Act allowed Medicare to negotiate prices for 10 high-cost drugs starting in 2026-but Humira isn’t included because it’s not yet on Medicare’s list. The FDA has increased inspections of Indian manufacturers, but staffing shortages limit impact. Patient groups are pushing for legislation to ban patent thickets and require full disclosure of manufacturing locations. Without major policy changes, the system will keep favoring profits over people.
